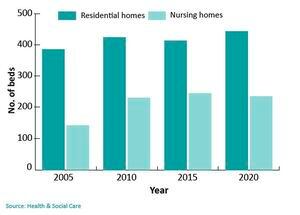
HSC reveals 6% drop in care home beds over last three years
AS GUERNSEY’S ageing demographic is starting to impact on care services it has been revealed that there has been a 6% drop in the number of care home beds over the last three years.
The care homes are currently full, and on Tuesday this week there were 27 people stuck at the Princess Elizabeth Hospital waiting for residential or nursing home beds to become available. A further four people were waiting for care in the community packages to be available so they could go back to their own homes. The build-up of hospital patients who would be better suited somewhere else is having a knock-on effect on operation cancellations.
There are currently 1,500 islanders on the operation waiting list, and that number goes up to 1,750 when private patients are included.
The latest statistics were revealed in the States by Health & Social Care president Al Brouard, in response to questions from Deputy John Gollop.
Deputy Brouard agreed that some people were in chronic pain, and he urged anyone in severe pain to make contact with their GP or the authorities.
‘Some of those patients I have no doubt will be in pain,’ he said.
‘It [the waiting list] has increased, we’ve managed to get the backlog down in the Soulsby years, it was down to about 600 to 700, so it has dramatically increased due to Covid.
‘I’m sure there are some people who are in very uncomfortable positions and it’s not a place we would like to be.’
Deputy Brouard said that bringing down the waiting list would take years, not months, and it was no longer possible to use UK hospitals because they were in an even worse position.
HSC is looking at building an eight-bed modular unit at the PEH which would be solely for knee and hip operations.
It is also considering extending the hours of the hospital, and whether more patients could be treated as day patients.
Deputy Neil Inder asked if there was data on the pressure that unvaccinated people were putting on the hospital.
He was given a commitment that Public Health would come back with a comprehensive answer, although Deputy Brouard added the caveat that it was ‘perfectly acceptable’ for people to not want to be vaccinated.
Deputy Liam McKenna wanted to know if other venues were being considered, such as the King Edward VII hospital, or the Castel hospital.
The response was that those options had been considered, but Deputy Brouard said the key issue was a shortage of staff.
‘So although we may have a beautiful building at King Edward VII and we make it all nice and clean for half a million pounds, we may not be able to staff it, and we would have staff split between two different sites.’





