Vaccine rollout faces ‘teething problems’ as hospitals come under pressure
Health Secretary Matt Hancock insisted manufacturers were producing as much vaccine as they could.

Family doctors are experiencing problems getting supplies of coronavirus vaccines for their patients, the Royal College of General Practitioners (RCGP) has warned.
The “teething problems” risked causing disappointment for vulnerable people who are at the front of the queue to receive the jabs, RCGP chair Professor Martin Marshall said.
The comments came as Health Secretary Matt Hancock launched the mass rollout of the Oxford/AstraZeneca Covid-19 vaccine to GP surgeries – but heard first-hand about the issues they face.
The need for the rapid rollout of the vaccine was underlined as hospitals across the UK faced rising numbers of seriously-ill patients.
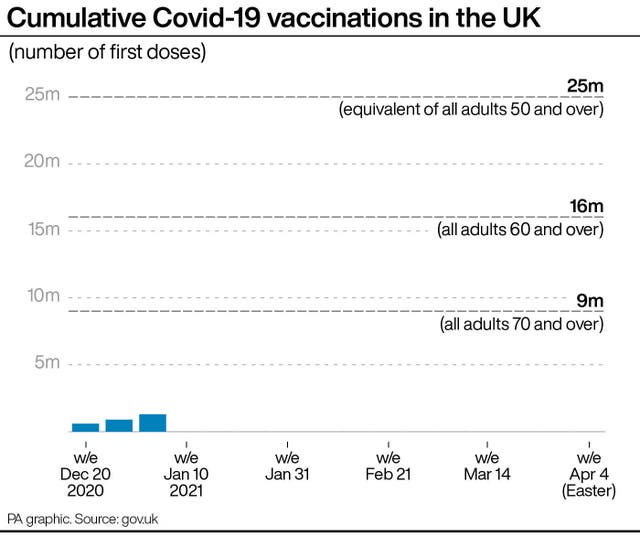
The jabs are being delivered to sites across the country as the Government attempts to offer a vaccine to more than 13 million people in the top four priority groups by mid-February – so far 1.3 million have received a jab.
Prof Marshall said GPs have already vaccinated hundreds of thousands of patients in the community using the Pfizer product and the Oxford vaccine should allow a greater number of people to be treated in a shorter space of time.
But he added: “Preparing for a vaccination clinic is no easy feat, it involves meticulous planning. Having to change these plans with little notice is frustrating and demoralising for GP teams – not to mention confusing and disappointing for patients.
“It’s vital that GPs and their teams on the ground, running vaccination clinics, are communicated with clearly and listened to – and that any concerns they have about the rollout taken seriously, so that they can be addressed.”
That message was underlined to Mr Hancock on a visit to the Bloomsbury Surgery in London, where an expected delivery of the Oxford vaccine was delayed.
Dr Ammara Hughes said Mr Hancock was “quite surprised actually to learn that we don’t know when all of our deliveries are coming, they’re very ad hoc”.
Appearing before MPs later, Mr Hancock said there were no delays in the supply of the vaccine, it was simply that producing it took time.
“The capacity constraint is the supply of the approved vaccine,” he said, rather than the ability to administer it to patients.
Meanwhile:
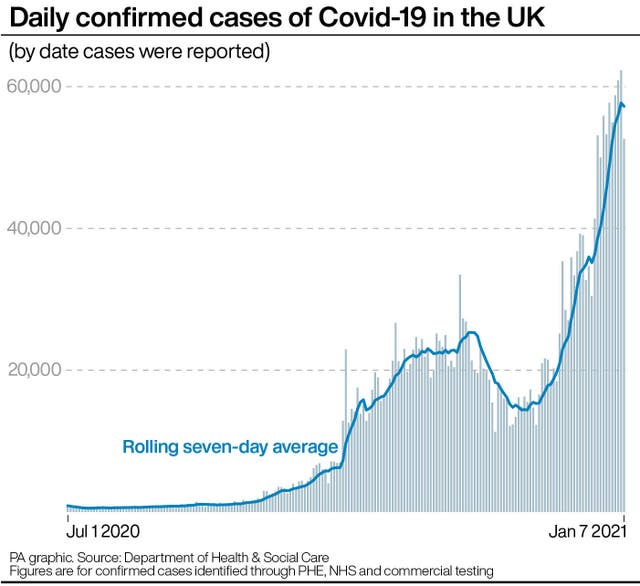
– A further 1,162 people died within 28 days of testing positive for Covid-19 as of Thursday – the highest daily reported total since April 21 – while there were 52,618 more lab-confirmed cases of coronavirus in the UK.
– Of the 269,886 people transferred to the NHS Test and Trace system in the week to December 30, 84.9% were reached, down from 86.4% in the previous week, and the lowest percentage since the week to October 28.
– Mr Hancock said he hoped all NHS staff would be offered the vaccine in the next few weeks, possibly even sooner than the February 15 target.

At St George’s Hospital in Tooting, south London, the trust has had to vastly expand intensive care capacity and move under-qualified staff to high dependency roles.
Dr Mark Haden, an emergency department consultant, said: “Everyone is working to the limit, to the threshold of what they’re able to.
“The hospital bed occupancy is very, very high, it has lots of Covid patients as inpatients at the moment. It’s very stressful for staff and that is starting to show.”
As of January 4, there were 30,451 people in UK hospitals with coronavirus, much higher than the April 12 peak of 21,684.
Rupert Pearse, professor of intensive care medicine and a consultant at the Royal London, said his own ICU staff are having to care for far more sick patients as he urged the public to heed the “stay at home” lockdown message.
He told BBC Radio 4’s Today programme there would usually be one fully-trained ICU nurse to one ICU patient but that was now being stretched to ratios of one nurse to three or even four patients.
“As intensive care doctors, we’re not sure how we can together deliver the quality of care that we need to,” he said.
Speaking on behalf of the Intensive Care Society, he said the problems are not just in London, but in other hospitals across the UK, and are not limited to ICU wards.
He added: “In essence, the healthcare available to all of us is not as good as it should be right now.”
The data showed that, even if the number of Covid patients grows at the lowest rate considered likely, and measures to manage demand and increase capacity, including opening the capital’s Nightingale hospital, are successful, the NHS in London will be short of nearly 2,000 general and acute (G&A) and intensive care beds by January 19.





