Combination of strikes and rise in flu and Covid ‘a perfect storm for the NHS’
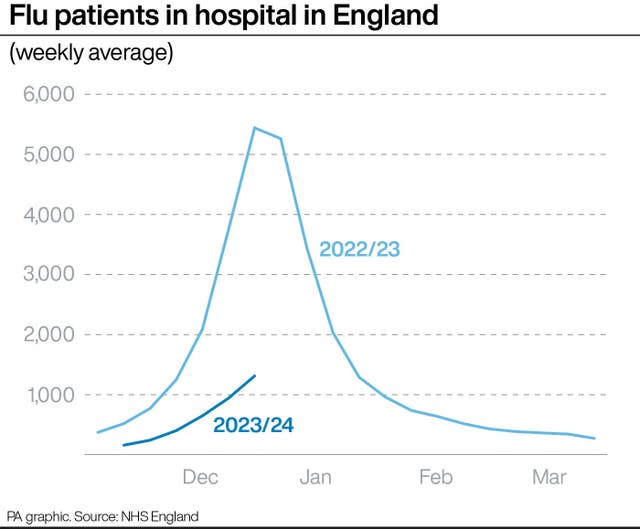
Figures published by NHS England on Friday show the number of flu patients jumped by more than a third over Christmas.

The “double whammy” of strikes on top of a rise in flu and Covid cases is a “perfect storm” heaping pressure on the NHS, a senior leader has said.
Sir Julian Hartley, chief executive of NHS Providers, which represents NHS trusts, warned that staff morale is low across the service and urged the Government and the British Medical Association (BMA) to end the industrial action.
Junior doctors are in the middle of a six-day strike, which is the longest walkout in the history of the health service.
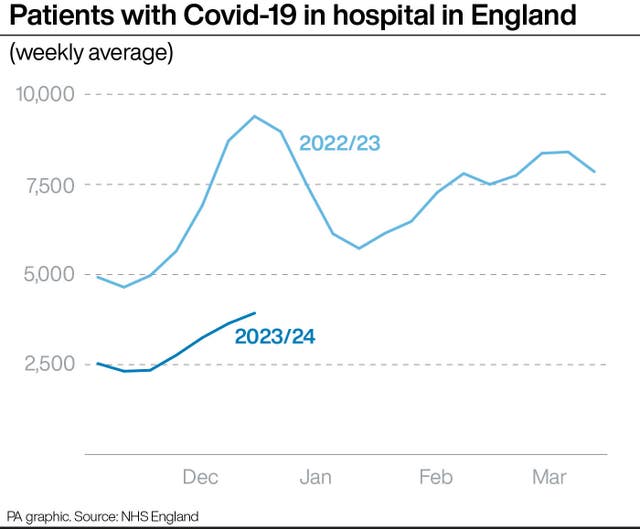
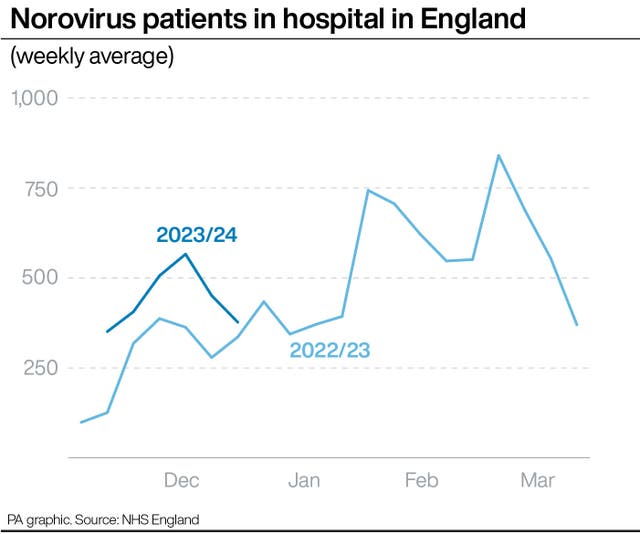
Covid-19 patient numbers are also continuing to rise, though norovirus levels appear to have peaked.
The figures give a snapshot of pressures on hospitals in the week to December 31, a time when the NHS was finalising its plans for dealing with the strike.
An average of 1,312 people were in hospital each day last week with flu, including 81 in critical care beds.
The total is up over a third (39%) from 942 the previous week, and more than double the 648 recorded a fortnight earlier.
It is the highest figure so far this winter but is still well below the number at this point a year ago – 5,441 – when the UK was in the middle of its worst flu season for a decade.
Sir Julian said of the new data: “The numbers show considerable pressure continuing to mount throughout the health system while hard-working teams pull out all the stops to give patients safe, high-quality care.
“The effects of a six-day strike by junior doctors this week, hard on the heels of a three-day stoppage before Christmas, will be felt right across an already hard-pressed NHS.
“In winter, guaranteed to be one of the busiest times of year for the NHS, a double whammy of walkouts on top of sustained pressure including more Covid-19 hospitalisations is a perfect storm.
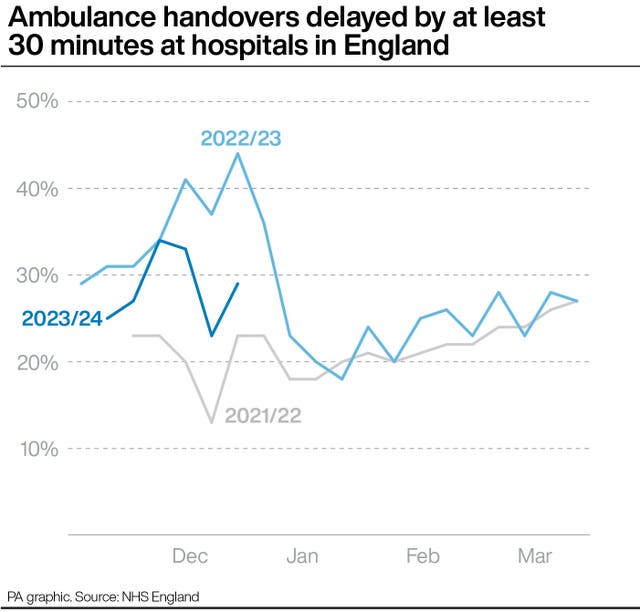
“Thanks to hard work and planning by trusts the NHS is reducing handover delays when people arrive at hospital in ambulances and cutting unnecessary hospital stays, enabling more patients to leave as soon as they’re well enough to do so.
“At the last count, stress, anxiety, depression and other mental illnesses were behind more than 27% of all sickness absences across the NHS.
“The Government and unions must act fast to settle this long-running dispute and prevent more walkouts for the sake of patients and staff.”
University Hospitals Plymouth NHS Trust declared a critical incident at 9am on Friday, “due to the sustained pressure across the hospital, with high attendances to our emergency department over the last three days”.
The latest industrial action by junior doctors began at 7am on Wednesday and runs until 7am next Tuesday.
It follows a 72-hour walkout in the week before Christmas.
Both strikes are part of a long-running dispute over pay, which has already seen 1.2 million inpatient and outpatient appointments rescheduled.
He added: “Although we have extensive preparations in place for strikes, and emergency care will continue to be prioritised, there is no denying the NHS has started the year in a very difficult position.
“This latest round of strike action will not only have an impact on this week but will have an ongoing effect on the weeks and months ahead, as we struggle to recover services and cope with heavy demand, but as ever, I would urge the public to get their flu and Covid vaccines if they are eligible, and continue to use 999 or A&E in an emergency, and 111 online for any other conditions.”
On Thursday, Health Secretary Victoria Atkins said the NHS “doesn’t just belong” to the BMA’s junior doctors’ committee.
She said the health service “cannot be switched on and off on whim” as she warned that the walkouts are having “very serious consequences” for patients and NHS workers.
Ms Atkins promised to start talks in 20 minutes if the strikes were called off.

But a row erupted after the BMA said the process was being “undermined” by the health service and suggested the requests were being made due to “political pressure”.
On Thursday, Prime Minister Rishi Sunak insisted that NHS leaders are “completely independent of Government” but added that they have his “backing” when making derogation requests.
More than 20 derogation applications have been submitted to the BMA, with the majority rejected. The union said NHS England and some trusts are refusing to provide evidence that they have undertaken steps to show they have “exhausted” all other sources of staffing before recalling medics.
NHS England bosses said in a letter that they will “continue to engage with the BMA in good faith to ensure the safety of patients” and that the BMA’s letter suggests the process for considering patient safety mitigations is “not working as well as it should” which they want to work to address.





