Waiting rooms ‘a thing of the past’, says Nightingale boss
The health service must “radically reorganise” to ensure it has Covid-19-free environments.

Hospital waiting rooms could become a thing of the past as the NHS changes how it works in response to the Covid-19 pandemic, the head of the first Nightingale hospital has said.
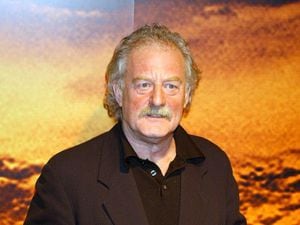
The NHS needs to “radically reorganise itself” in order to provide some coronavirus-free hospitals or environments, Professor Charles Knight, seconded to run the NHS Nightingale Hospital in London’s ExCeL Centre, said.
Many hospital appointments have been conducted on the phone or over video call, which will probably be a permanent feature of hospitals going forward, he added.
During a Royal Society of Medicine webinar on the creation of the Nightingale Hospital, the hospital boss, who is also a consultant cardiologist, described how some patients have become “averse” to seeking help for non-Covid-19 medical problems, adding “this has to stop”.
He said the Nightingale hospital was created in a “remarkably short” period of time, adding: “I don’t think there’s many private-sector companies that could have, or indeed have, responded to the pressures of Covid in the way we [the NHS] did. I don’t think Ocado has quite got its delivery sorted out as quickly as we sorted out the Nightingale.”
Modelling suggested that London may have needed as many as 7,500 intensive care beds for Covid-19 patients – a steep rise from the 799 in situ.
He added that it was “wonderful” the Nightingale had not been needed on such a large scale, but admitted that it would have been “difficult” to staff all of the beds in the hospital.
“And I think we would have had to find a way, we would have had to stretch skilled staff, supporting them with less skilled staff, to try and make that work because the alternative was unthinkable,” he said.
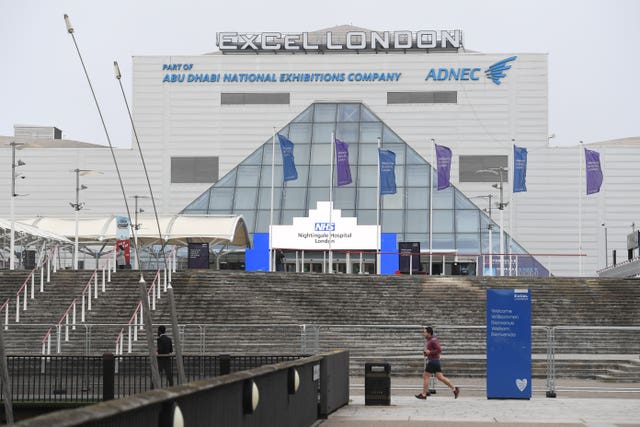
Prof Knight said that watching the rows and rows of beds set up at the conference centre “felt apocalyptic”.
“When we first came here, and we looked at these vast halls and we saw the beginnings of the bed bays being rolled out – it was a profoundly moving, a really awe-inspiring and horrific moment, because if you imagined all those beds being full of patients – it was like the apocalypse,” he said.
“The sense of scale is unimaginable.”
He said it was agreed that the Nightingale was a “temporary phenomenon” and it could offer support as an insurance policy for a possible second peak, and as a “bridge” to help the health service get back to its usual business.
“And there is an increasing need for London, and the rest of the UK, to get back to some degree of normal operating so that we are not losing patients from heart disease and cancer and other important conditions that would usually get treated,” he said.
“And the two reasons we haven’t been able to do that are because our intensive care units are full of [Covid-19] patients. And also, because the public has become very understandably very averse to going into a hospital.
“There’s increasing evidence that people are not taking the notice they usually would have of chest pain, and then presenting very late with much bigger myocardial infarctions (heart attacks) or even an increased risk of dying at home, cardiac arrest. That has to stop.”
Part of a “bridging” phase could see Covid-19 patients “decanted” to the Nightingale so hospitals could become “essentially Covid-free”.
Prof Knight added: “It’s quite clear that the health service, regardless of the Nightingales, will need to radically reorganise itself in order to provide some Covid-free hospitals or environments where patients are not at risk of infection and can have the confidence that they can get in, and be treated, and leave, without contracting the disease.”
He highlighted the work at St Bartholomew’s Hospital in London, which has managed to create a Covid-19-free environment so it can still deliver life-saving care for heart patients.
Pre-operation screening for patients includes two swabs at different periods of time, symptom questionnaires and a CT scan of the chest, before patients can have surgery.
So far 100 patients with urgent need for heart surgery – including bypass, aortic dissection and valve replacements – have had surgery without contracting Covid-19.
“The other important changes I’m sure everyone will know is the very rapid move to telephone and video outpatients. I think that has to and will be a prolonged and probably permanent feature of hospitals going forward,” said Prof Knight.
“The hospital outpatient waiting room is probably a thing of the past and we shouldn’t have it back.”
He added: “We can take pride in what’s been achieved in terms of the flexibility of the response across the whole country. And also, to learn from that to be more agile in the future and not go back to quite the sort of level of bureaucracy that we used to deal with.”